Table of Contents
Common Joint Pathologies and Etiology of Symptoms
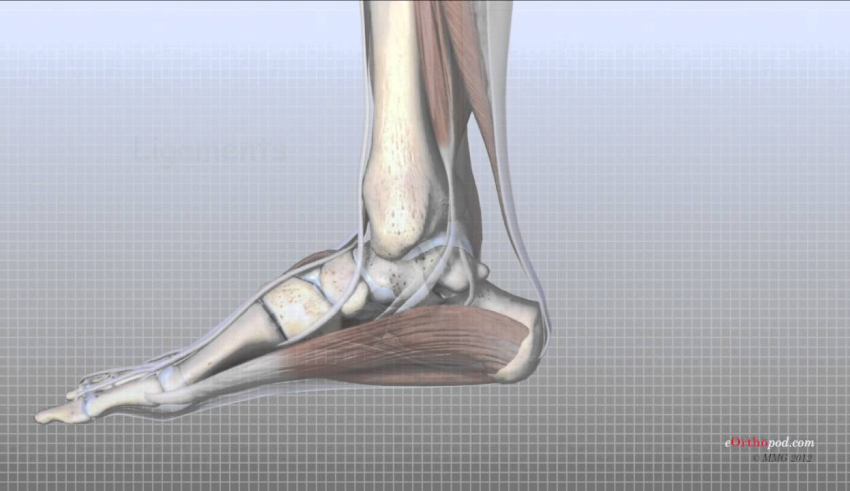
Pathologies such as rheumatoid arthritis (RA); juvenile rheumatoid arthritis (JRA); degenerative joint disease (DJD); and acute joint reactions after trauma, dislocations, or fractures affect the Fractured Ankle Management. Post-immobilization contractures and adhesions develop in the joint capsules and surrounding tissues any time a joint is immobilized in a cast or splint, typically after dislocations and fractures.
Rheumatoid arthritis.
Joint pathology of foot and ankle as the result of RA commonly affects the forefoot early in the disease process, later the hindfoot, and least frequently, the ankle. Involvement may occur in the MTP, subtalar, talocrural joints of the foot, leading to instabilities and painful deformities, such as hallux valgus and subluxation of the metatarsal heads, that increase with the stress of weight bearing. Tendon rupture of foot and ankle musculature also may occur as the result of chronic inflammation and contribute to deformity.
Degenerative joint disease (DJD) and joint trauma.
Degenerative symptoms occur in joints that are malaligned or repetitively traumatized, and acute joint symptoms are often seen in conjunction with ankle sprains, chronic instability, or fracture. Post-traumatic arthritis leading to DJD is by far the most common type of arthritis that affects the ankle, accounting for approximately 80% of all ankle arthritis. In contrast, primary osteoarthritis, a common type of arthritis in the hip and knee, is rare in the ankle, even in the older adult population.105
Post-immobilization stiffness. Contractures and adhesions in the capsular tissues leading to joint hypomobilities as well as in the surrounding periarticular tissues may occur
any time the joint is immobilized after a fracture or surgery.
Symptoms commonly affect the MTP joint of the great toe, causing pain during terminal stance so that there is a shorter stance and lack of smooth push-off.
Common Impairments and Functional Limitations/Disabilities
In RA, many of the following impairments and deformities occur with progression of the disease.18,92 With DJD and post-immobilization stiffness, only the affected joint or joints are limited.16 Functional limitations and disabilities occur primarily as a result of loss of weight-bearing abilities.
Fractured Ankle Restricted motion
When symptoms are acute, the patient experiences swelling and restricted, painful motion, particularly during weight-bearing activities. When symptoms are chronic, there is restricted motion, decreased joint play, and a firm capsular end-feel in the affected joint.
Decreased mobility in the proximal and distal tibiofibular joints.
Restricted accessory motion in these joints usually occurs with periods of immobilization and limits ankle and subtalar joint motion.
Talocrural joint.
Passive plantarflexion is more limited than dorsiflexion (unless the gastrocnemius–soleus muscle group also is shortened, in which case dorsiflexion is limited accordingly
Subtalar and transverse tarsal joints.
Progressive limitation of supination develops until eventually the joint fixes in pronation with flattening of the medial longitudinal arch. The close-packed position of the tarsals (supination) becomes more and more difficult to assume during the terminal stance (push-off) phase of gait.
MTP joint of the large toe.
Gross limitation of extension and some limitation of flexion develop; the rest of the MTP joints are variable
Lack of extension restricts the terminal stance phase of gait with an inability to rock up onto the metatarsal heads. This exacerbates the pronation posture and inability to supinate the foot during push off in gait
Common deformities
Deformities occur due to a variety of factors including but not limited to muscle imbalances,faulty footware, trauma, and heredity.
Hallux valgus.
This deformity in the great (large) toe develops as the proximal phalanx shifts laterally toward the second toe. Eventually the flexor and extensor muscles of the great toe shift laterally and further accentuate the deformity. The bursa over the medial aspect of the metatarsal head may become inflamed and the bone hypertrophies, causing a painful biunion.
Hallux rigidus.
Narrowing and eventual obliteration of the first MTP joint space occur with progressive loss of extension. This affects terminal stance by not allowing the foot to roll over the metatarsal heads and great toe for normal push-off. Instead, the individual turns the foot outward and rolls over the medial aspect of the large toe. This faulty pattern accentuates hallux valgus and foot pronation, and usually the MTP joint is quite painful.
Dorsal dislocation of the proximal phalanges on the metatarsal heads.
If this occurs, the fat pad, which is normally under the metatarsal heads, migrates dorsally with the phalanges, and the protective cushion on weight bearing is lost, leading to pain, callus formation, and potential ulceration.
Claw toe (MTP hyperextension and IP flexion) and hammer toe (MTP hyperextension, PIP flexion, and DIP hyperextension).
These result from muscle imbalances between the intrinsic and extrinsic muscles of the toes. Friction from shoes may cause calluses to form where the toes rub.
Muscle weakness and decreased muscular endurance.
Inhibition resulting from pain and decreased use of the extremities lead to impaired muscle function.
Impaired balance and postural control
The sensory receptors in the ankle joints and ligaments, as well as in the muscle spindles, provide important information for posture and movement, known as the ankle strategy. The ankle strategy is used in balance control during perturbations. Faulty feedback and balance deficits occur when there is instability, muscle impairments, or arthritis.
Increased frequency of falling.
Impaired balance may lead to frequent falling or fear of falling and thus restrict community outings.
Painful weight bearing.
When symptoms are acute, weight-bearing activities are painful, preventing independent ambulation and causing difficulty in rising from a chair and ascending and descending stairs.
Gait deviations.
If the patient experiences pain during weight bearing, there is a short stance phase, reduced single limb support, and decreased stride length on the side of involvement. Because of the restricting motion and loss of effective plantarflexion and supination in the arthritic foot, as well as pain in the forefoot area under the metatarsal heads, push-off is ineffective during terminal stance. Little or no heel rise occurs; instead, the person lifts up the involved foot
Decreased ambulation.
Because of decreased ankle and foot mobility and resulting decreased length of stride,distance and speed of ambulation are decreased; the person may require use of assistive devices for ambulation. If pain, balance, or restricted motion is severe the person will be unable to ambulate and, therefore, requires a wheelchair for mobility.
Joint Hypomobility: Fractured Ankle Management— Protection Phase
Educate the Patient and Provide Joint Protection in Fractured Ankle Management
Teach a home exercise program at the level of the patient’s abilities. Teach the patient to be aware of signs of systemic fatigue (especially in RA), local muscle fatigue, and joint stress, and how to modify exercises and activities to remain active within safe levels. Emphasize the importance of daily ROM, endurance activities, and joint protection Fractured Ankle Management
Decrease Pain
In addition to physician-prescribed medication, intra articular injections of corticosteroids, or nonsteroidal anti-inflammatory medications, and therapeutic use of modalities the following are used to manage painful symptoms.
Manual therapy techniques for Fractured Ankle Management. Gentle grade I or II distraction and oscillation techniques may inhibit pain and move synovial fluid for nutrition within the involved joints.
Orthotic devices. Orthotics and well-constructed shoes help protect the joints by realigning forces and providing support from faulty foot postures.45,62,65 Such support has been shown to decrease pain and improve functional mobility. Splinting or bracing may also be used to stabilize an arthritic joint.
Maintain Joint and Soft Tissue in Fractured Ankle Management
Mobility and Muscle Integrity
Passive, active-assistive, or active ROM. It is important to move the joints as tolerated. If active exercises are tolerated they are preferred because of the benefits of muscle action.
Aquatic therapy. Aquatic therapy is an effective method of combining nonstressful buoyancy-assisted exercises with therapeutic heat.
Muscle setting. Apply gentle multiangle muscle-setting techniques in pain-free positions and at an intensity that does not exacerbate symptoms.
Joint Hypomobility: Management—Controlled Motion and Return to Function Phases
Examine the patient for signs of decreased muscle flexibility joint restrictions, muscle weakness, and balance impairments. Initiate exercises and mobilization procedures at a level appropriate for the condition of the patient.
PRECAUTIONS WITH RA in Fractured Ankle Management:
Modify the intensity of joint mobilization and stretching techniques used to counter anyrestrictions because the disease process and use of steroid therapy weaken the tensile quality of the connective tissue
Increase Joint Play and Accessory Motions
Joint mobilization techniques.
In Fractured Ankle Management Determine which articulations are restricted owing to decreased joint play, and apply grade III sustained or grade III and IV oscillation techniques to stretch the limitations. (read more….)